Pain | Pathway and Analgesics (NSAIDs, Opioids, Antidepressants, and Anticonvulsants)
Dr Matt & Dr Mike・45 minutes read
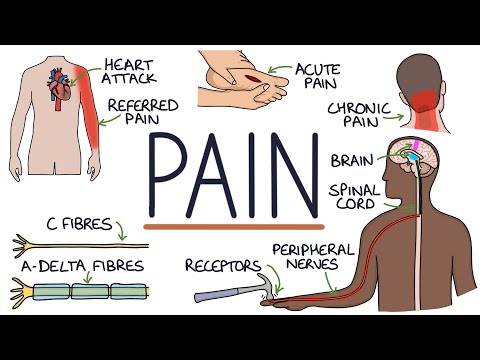
Pain is a complex sensory and emotional experience linked to various stimuli, with distinct pathways for transmitting fine touch and pain signals in the brain. Different types of pain, such as nociceptive and neuropathic, require specific management strategies ranging from NSAIDs and opioids for acute pain to antidepressants and anticonvulsants for chronic pain.
Insights
- Pain is a complex sensory and emotional experience linked to tissue damage, transmitted by A delta and C fibers, with A delta fibers responsible for sharp, localized pain and C fibers for diffuse, slow pain.
- Fine touch and pain signals follow distinct pathways in the spinal cord, with A delta fibers synapsing early and providing specific pain sensations, while C fibers branch out to the brain's limbic system, influencing emotional responses and wakefulness.
Get key ideas from YouTube videos. It’s free
Recent questions
What are the two main types of fibers responsible for transmitting pain signals?
A delta fibers and C fibers.
Related videos
Zero To Finals
Understanding The Causes of Pain and Pain Management
Armando Hasudungan
Nociceptors - An Introduction to Pain

Armando Hasudungan
PAIN! Physiology - The Ascending Pathway, Descending Pain Pathway and the Substantia Gelatinosa

The Infographics Show
50 Insane Facts About Pain

Talks at Google
Breakthrough with Healing Chronic Pain | Howard Schubiner | Talks at Google
Summary
00:00
Pathways of Pain and Touch Signals
- Pain is defined as an unpleasant sensory and emotional experience linked to tissue damage, as per the International Association for the Study of Pain.
- Pain differs from other sensory experiences like touch or sight due to its emotional component significantly affecting the experience.
- Triggers for pain include mechanical, thermal, and chemical stimuli, which are picked up by free nerve endings acting as receptors.
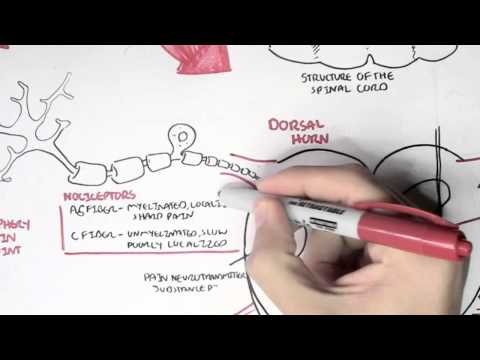
- Two main types of fibers, A delta fibers, and C fibers, are responsible for transmitting pain signals to the brain, with A delta fibers sending fast signals for sharp pain and C fibers sending slow signals for dull pain.
- Pain can be triggered by high threshold mechanical, mechanical thermal, and poly modal receptors, each responding to specific stimuli.
- The spinal cord's white matter acts as pathways for sensory input, with the dorsal column medial lemniscus pathway carrying fine touch signals to the brain.
- The spinothalamic tract is responsible for transmitting pain and temperature signals to the brain, following a different pathway than fine touch signals.
- Fine touch signals follow a three-neuron chain from the spinal cord to the thalamus and then to the cortex for processing.
- In contrast, pain signals from nociceptors follow a separate pathway, synapsing at the medulla before reaching the thalamus and then the cortex.
- Understanding the distinct pathways for fine touch and pain signals is crucial for comprehending how sensory information is processed in the brain.
18:16
"Pain Transmission and Modulation in Neurology"
- A signal transmission process involves A delta and C fibers, entering through the dorsal nerve root into the dorsal gray horn.
- A delta fibers synapse early in the dorsal gray horn, specifically in the first two layers, before crossing over to the lateral white matter.
- The A delta fiber pathway bypasses the medulla, going directly to the thalamus for sensory awareness, particularly for pain perception.
- Pain signals from A delta fibers follow a three-neuron chain, involving synapses at the dorsal gray horn, crossing over, and reaching the thalamus before the cortex.
- A delta fibers provide localized and specific pain sensations, distinct from C fibers, which offer diffuse and slower pain signals.
- C fibers, slower at 0.5 to 1 meter per second, branch out to the reticular system and limbic system in the brain, affecting wakefulness and emotional responses.
- Pain modulation occurs peripherally and centrally through various neurotransmitters and chemicals like glutamate, substance P, potassium, bradykinin, and prostaglandins.
- Inflammation, linked to pain, releases chemicals that stimulate pain receptors and lower pain thresholds, influencing the perception of pain.
- The Pain Gate Theory suggests that stimulating touch fibers can inhibit pain signals at the spinal cord level, limiting the transmission of pain to the brain.
- Brown-Séquard syndrome, resulting from a hemi-lesion in the spinal cord, can lead to differential touch and pain perception on the contralateral side below the level of injury.
37:03
Understanding and Managing Chronic Pain Syndromes
- Brown-Sicard syndrome involves pain pathways where injury below the level of injury on the same side does not reach the brain, causing ipsilateral pain.
- To test for Brown-Sicard syndrome, run an ice cube up a limb and ask the patient to identify temperature and touch sensations.
- The endogenous opioid system modulates pain by releasing chemicals like endorphins and dynorphins to reduce pain signals.
- Acute pain lasts less than three months, while chronic pain persists beyond three months, often resulting from unmanaged acute pain.
- Nociceptive pain is associated with tissue damage, while neuropathic pain is chronic and often unrelated to tissue damage.
- Inflammation triggers acute nociceptive pain, reducing pain thresholds and increasing pain signals.
- NSAIDs like aspirin, ibuprofen, celecoxib, and acetaminophen block prostaglandins to reduce inflammatory pain.
- Opioids like morphine and fentanyl mimic endogenous opioids but are less effective for chronic pain due to various reasons.
- Central sensitization can occur, leading to hyperalgesia and allodynia, where pain signals are amplified without external stimuli.
- Chronic pain, termed neuropathic, lacks an underlying cause, requiring management to reduce pain stimuli rather than addressing a specific trigger.
56:15
Managing Chronic Pain: Alternatives to Morphine
- Morphine is typically used for acute, severe pain lasting around three to five days due to its addictive properties and limited effectiveness for chronic pain.
- For chronic pain, antidepressants like tricyclic antidepressants and serotonin-specific reuptake inhibitors, as well as anticonvulsants, are commonly used to target the descending opioid system involving serotonin and noradrenaline neurotransmitters.
- Antidepressants like tricyclic antidepressants and serotonin-specific reuptake inhibitors inhibit reuptake mechanisms, keeping neurotransmitters in the synapse longer to increase the release of endogenous opiates, while also blocking sodium channels on pain neurons to prevent pain signal transmission.
- Anticonvulsants like gabapentin, also used for chronic pain, work as calcium channel blockers to inhibit the release of pain neurotransmitters, alongside non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin and ibuprofen, and opioids such as morphine and fentanyl, which mimic the endogenous opioid system to block pain transmission and alter pain perception in the brain.




