Narrated Cardiac Pharm 1220 F24
SLCC Med Surg Videos・48 minutes read
Thrombogenesis and hemostasis play essential roles in clot formation and cessation of blood flow after vessel injury. Heparin and warfarin are commonly used anticoagulants that require careful monitoring to maintain therapeutic levels and prevent adverse effects.
Insights
- Thrombogenesis is the formation of blood clots to prevent blood loss from vessel injury, while hemostasis involves stopping blood flow through mechanisms like vasoconstriction and platelet plug formation.
- Heparin and warfarin are essential anticoagulants that prevent clot formation by inhibiting clotting factors or blocking vitamin K synthesis, respectively; monitoring PT and PTT for heparin and PT/INR for warfarin helps maintain therapeutic levels and prevent complications.
Get key ideas from YouTube videos. It’s free
Recent questions
What is thrombogenesis?
The formation of blood clots to prevent blood loss.
Related videos

Ninja Nerd
Antiplatelet, Anticoagulant, Thrombolytic Agents
Thrombosis Adviser
Coagulation Cascade Animation - Physiology of Hemostasis

Zero To Finals
Understanding Deep Vein Thrombosis (DVT)

YAKEEN
BODY FLUIDS AND CIRCULATION in 1 Shot: FULL CHAPTER COVERAGE (Theory+PYQs) || Prachand NEET 2024

Amoeba Sisters
Punnett Squares and Sex-Linked Traits (UPDATED)
Summary
00:00
Blood Clot Formation and Prevention Mechanisms
- Thrombogenesis is the formation of blood clots, a normal body defense mechanism to prevent blood loss from vessel injury.
- Plasminogen, an inactive protein, becomes part of the clot during clot formation and is activated to produce plasmin, an enzyme that breaks down the clot's fibrin meshwork.
- Imbalance between thrombogenesis and thrombolysis can lead to thrombotic or bleeding disorders.
- Hemostasis involves mechanisms like vasoconstriction and platelet plug formation to stop blood flow and repair vessel tears.
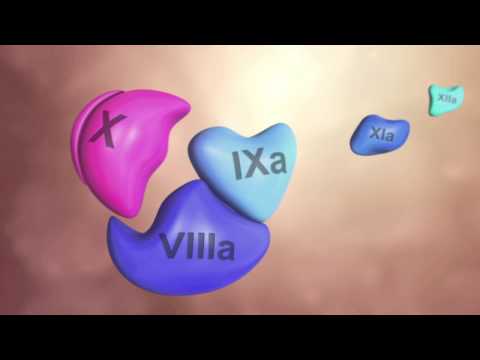
- The intrinsic pathway involves clot formation inside the blood vessel, while the extrinsic pathway forms clots outside the vessel.
- Anti-platelet drugs alter platelet aggregation, anticoagulants interfere with clotting cascade and thrombin formation, and thrombolytic agents break down clots.
- Heparins, like enoxaparin, inhibit clotting factors and prevent thrombus formation.
- Warfarin, an oral anticoagulant, prevents the synthesis of factors dependent on vitamin K for synthesis.
- Prothrombin time (PT) and partial thromboplastin time (PTT) are used to monitor coagulation disorders and the effectiveness of heparin and warfarin therapy.
- Heparin, administered parenterally, prevents clot extension and formation, but does not break down existing clots; contraindications include thrombocytopenia and active bleeding.
19:51
"Anticoagulant Therapy: Heparin and Warfarin Essentials"
- Therapeutic levels of heparin should be between 55 and 60, achieved by multiplying the base level by 1.5 to 2 times.
- It takes 6 to 8 hours to reach a steady state with heparin, after which regular testing should commence.
- Heparin should be administered via a dedicated IV pump to avoid interactions with other drugs.
- Double-check calculations with another care provider when dosing heparin to prevent adverse effects.
- Subcutaneous injections of heparin should not be massaged or aspirated to reduce the risk of hematoma formation.
- Low molecular weight heparin, like enoxaparin or Lovenox, has a longer half-life than regular heparin and is usually given once or twice a day.
- Warfarin competitively blocks vitamin K to prevent clotting factors activation, affecting factors II, VII, IX, and X.
- Warfarin is metabolized in the liver, excreted in the bile, and should not be used during pregnancy due to fetal warfarin syndrome risks.
- The antidote for warfarin is vitamin K, and patients should maintain a consistent intake of vitamin K-rich foods to stabilize therapeutic levels.
- Monitoring the PT and using the International Normalized Ratio helps ensure the effectiveness of warfarin therapy over time.
38:27
Optimizing Warfarin Therapy for Anticoagulation Management
- Warfarin is used to measure therapeutic levels, standardizing PT and control times.
- Prophylaxis aims for PT to be 1.4-1.6 times normal, resulting in an INR of 2-3.
- Patients with mechanical heart valves require higher anticoagulation levels.
- Monitoring PT regularly is crucial for maintaining therapeutic anticoagulation.
- Patients should take medication at the same time daily for consistent results.
- INR range provides flexibility in PT monitoring.
- Patients should avoid aspirin and ibuprofen due to additive effects on clotting.
- Education on monitoring for bleeding symptoms is essential for patients.
- Thienopyridines like clopidogrel inhibit platelet aggregation, prolonging bleeding time.
- Clopidogrel is absorbed well in the GI tract, with steady state achieved in 3-7 days.
56:33
Assessing and Monitoring Risks in Thrombolytic Treatment
- Evaluating for atherosclerotic events risk is crucial.
- Monitoring for bruising and notifying patients about excessive bruising is essential.
- Neutropenia and increased infections are signs to watch for.
- Assessing liver function and CBC levels is necessary.
- Taking thrombolytic agents with food reduces adverse GI effects.
- Tenecteplase and alteplase are thrombolytic agents binding to fibrin in clots.
- Tenecteplase is easier to use than alteplase for acute myocardial infarctions.
- Monitoring for bleeding is crucial during thrombolytic agent administration.
- Baseline labs like PTT, INR, platelet counts are essential before treatment.
- Lipid profile tests after fasting for 12 hours are vital for assessing cholesterol levels.
01:19:49
Managing Nitroglycerin: Monitoring, Dosage, and Absorption
- Monitoring blood pressure is crucial due to potential reflex tachycardia following a drop in blood pressure.
- Patients are advised to lie or sit down to reduce the risk of falls and decrease oxygen demands.
- Nitroglycerin dilates arteries, reducing systemic vascular resistance and arterial pressure, thus decreasing the heart's workload and oxygen needs.
- Tolerance to nitroglycerin can develop, so starting with a small dose and removing patches for 10-12 hours daily can help minimize this.
- Sublingual absorption of nitroglycerin is rapid, but dry mouth can hinder absorption.
- Transdermal absorption increases with exercise, elevated external temperatures, or application to broken skin.
- Nitroglycerin has a first-pass effect, is metabolized in the liver, and excreted in urine. Storage in a dark bottle is essential to prevent deterioration.




